Sick Enough by Dr. Jennifer L. Guadiani is a great resource both for those experiencing an eating disorder and for those who love them.
Through breaking down complex medical topics into bite size pieces, this book helps readers understand the real, medical complications of eating disorders, while addressing barriers to treatment.
Dr. Jennifer L. Gaudiani, author of Sick Enough, is a board certified-internal medicine doctor specializing in the treatment of eating disorders. She is also the founder of the Gaudiani Clinic: an outpatient medical practice specializing in the treatment of eating disorders. Before that work, she worked at ACUTE Center for Eating Disorders and Severe Malnutrition, which treats people with extreme medical complications of eating disorders. Dr. Gaudiani has spoken on this topic worldwide, is published in scientific journals and much more.
All people with an eating disorder deserve care and treatment. This is a simple but powerful idea that is reinforced again and again throughout Sick Enough.
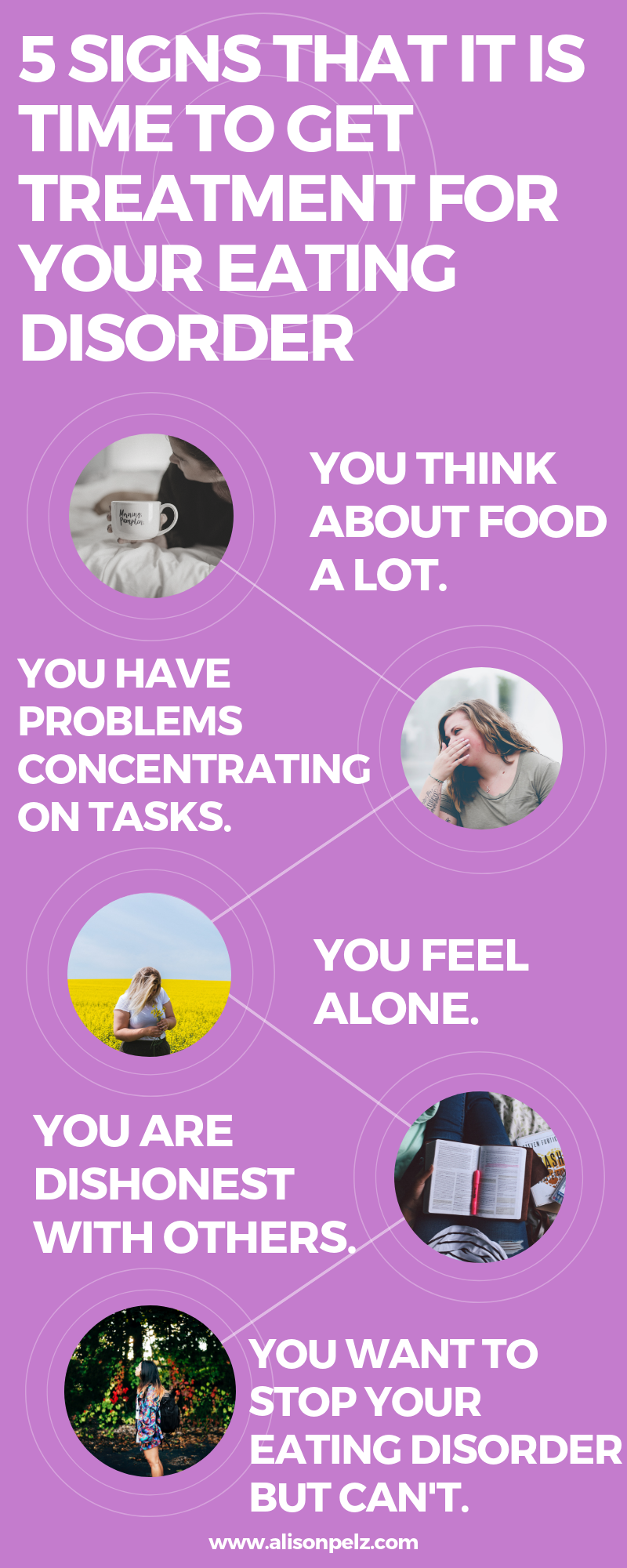
Maybe you’ve thought your eating disorder “isn’t that bad,” or felt like you don’t “look” like you have an eating disorder.” This happens for varying reasons. Many folks who experience eating disorders feel or are made to believe that their disorder isn’t legitimate because they don’t fit the mold of “type” of people who get eating disorders. Or they’ve experienced their eating disorder minimized by well-meaning but underinformed mental health providers, doctors, and even family members.
Eating disorders affect people’s physical health, not just their mental health. It is important to know how being under fed and under nourished (even if you experience binge eating or bulimia) can affect the digestive track, mood, muscle tone and much more.
Yes, Gaudiani emphasizes, all who experience eating disorders are “Sick Enough” to warrant treatment.
Why read Sick Enough?
In Part I, “Not Enough Calories” Gaudiani initiates an important discussion on what happens to the mind and body when enough calories are not consumed over a period of time–with intentionally dramatic and jarring chapter titles like “30,000 Foot View: What Happens When You Starve Yourself?,” and “Going Into Hibernation and The Empty Tank.”
Gaudiani starts off by introducing the reader to the “cave person brain” aka the part of our brain that regulates some of the most basic bodily functions and what it does to keep us alive when the body is underfed. She illustrates the devastating effects (regardless of body size) that not getting enough calories can have on both physical health and psyche–no matter if it’s due to dieting, an eating disorder, or food insecurity.
Examining Unexplored Biases in Sick Enough:
Refeeding syndrome*, which describes the condition of introducing food too much too quickly to someone who has been malnourished, is something many dietitians, myself included, are instructed to the point of repetition to be cautious of.And while it can present real danger to patients, Gaudiani takes time to explore how the more common, equally dangerous condition of “underfeeding” is historically overlooked in eating disorder treatment, largely due to weight bias in the field.
Genetic variability is another concept Gaudiani explores within Sick Enough. As clinicians we are often baffled when a client who suffers from a severe eating disorder gets their lab work back and it all looks “normal.”Many providers can also be shocked to learn a client has lost their menstrual cycle without appearing to have lost much weight. In exploring how different people react to inadequate food intake, Dr.Gaudiani gives a thorough discussion on genetic variability as a reason we see things like this.
The book’s final section dives into the relationship and intersection of eating disorders and different gender identities, sexual orientations, ages, and chronic health conditions like diabetes. Gaudiani wraps it all up by providing a brief discussion on caring for those who have long and enduring eating disorders, and those who decline eating disorder care.
Throughout the book Dr. Gaudiani weaves in critical discussions on weight bias and weight stigma, and how they function as barriers to accurate diagnosis, treatment and care, as well as diving into and deconstructing pseudo science popularized by diet and wellness culture.
Sick Enough may be a challenging read at times–it goes into detail about some of the more rare medical complications of eating disorders which feel daunting to the reader.
While Gaudiani does her best at acknowledging the complexities of eating disorders within various identities–something historically excluded from the eating disorder treatment space– most of these sections are brief and not in-depth. Missing entirely is a discussion on neurodiversity and how it can complicate eating disorders and eating disorder treatment–RDs for Neurodiversity and Eating Disorder and Autism Collective are resources outside the scope of this book to begin learning more about neurodiversity and how it impacts eating disorders.
Who is Sick Enough for?
- Medical professionals
- Those who are experiencing an eating disorder and their loved ones
- Caregivers
Sick Enough is loaded with invaluable vignettes and metaphors that can be used with clients–as a therapist and dietitian it helps me communicate and collaborate more effectively with my client and the whole treatment team, as well as helping me advocate for clients in spaces that aren’t eating disorders friendly.
If you are a clinician wanting to learn more about eating disorders and their treatment, sign up here to receive free eating disorder resources in your inbox.
As a therapist who is also a dietitian, I can help you understand what is going on from both angles. If you are in Texas and interested in working with me, click here to fill out a contact form. I would love to support you and your child on your journey to health.
*Please consult your doctor if you think you have an eating disorder before beginning treatment.
Cover Image courtesy of Taylor & Francis, 2019