Keeping your eating disorder recovery front and center during the COVID-19 pandemic may be the furthest thing from your mind, given that we are all adjusting to a new way of life, navigating uncertainty, and dealing with loss and worries about our health, to name a few pressing issues.
Here are some tips to help you maintain and even thrive with your eating disorder recovery during this unusual and trying time:
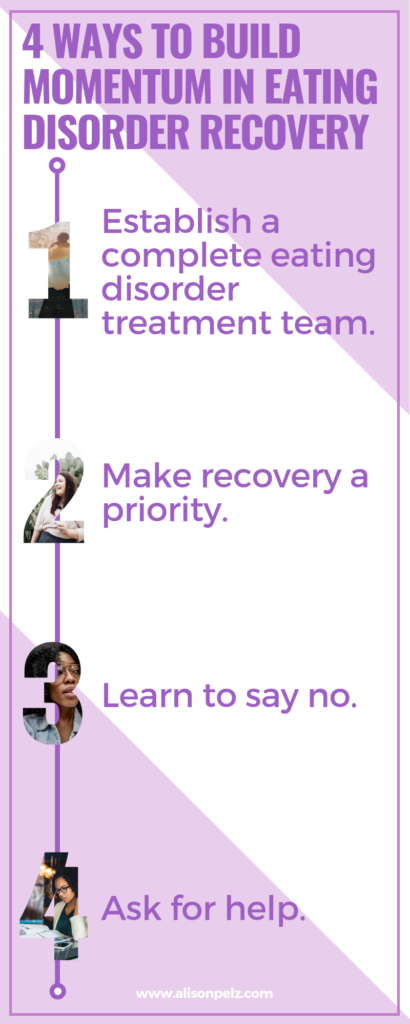
1. Keep eating disorder recovery on the priority list during COVID-19.
Of course, your priorities have shifted in the wake of COVID-19. First and foremost, you are dealing with the stress of this health crisis. Time and energies have shifted because you are adjusting to a new way of life, including being cooped up in the house; working or schooling from home; health risks; and isolation.
While these changes may seem overwhelming at times, know that you can tend to your eating disorder recovery during this time. As with everything right now, your recovery may look different than usual, and that’s okay.
2. Stay in touch with your eating disorder treatment team.
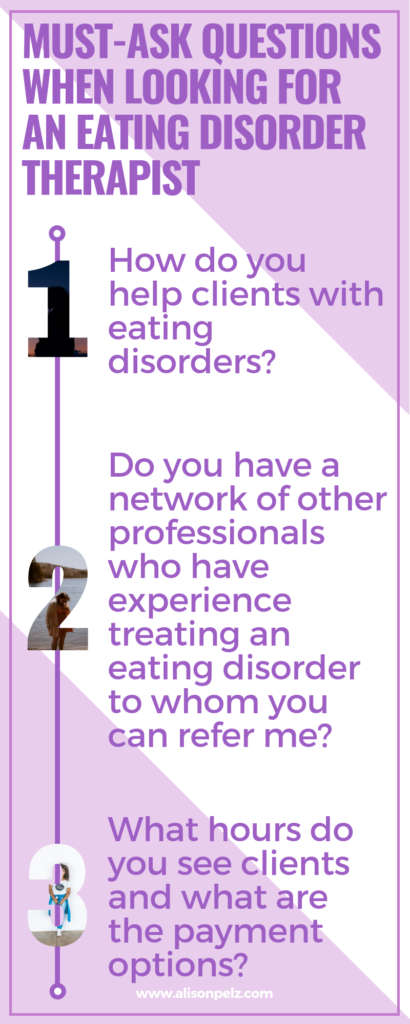
If you have not checked in with your treatment team—including your therapist, dietitian, and doctor—that may be a good first step. Most clinicians are conducting telehealth appointments, which may include video conferencing, telephone, email, and FaceTime appointments. Telehealth may feel a little daunting at first, but I am finding it to be an effective way to continue to support clients with eating disorders.
If you don’t have an eating disorder treatment team, read more here about how to find eating disorder services in your area.
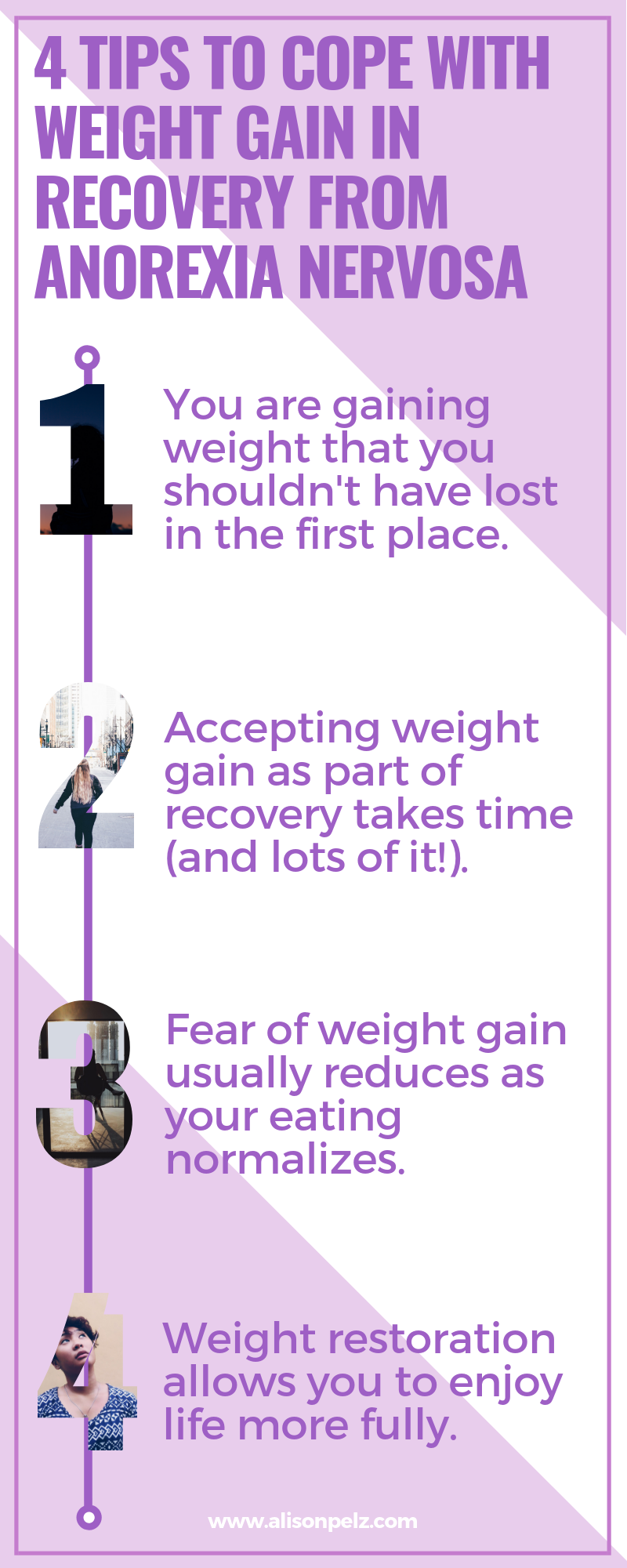
3. Accept that your eating may be different during COVID-19, and that’s okay.
Changes in food accessibility, cooking at home vs. eating out, living situation, mood fluctuations, and activity level can all contribute to changes in eating patterns. Talk with your treatment team about any changes you have noticed with your eating as well as alcohol consumption.
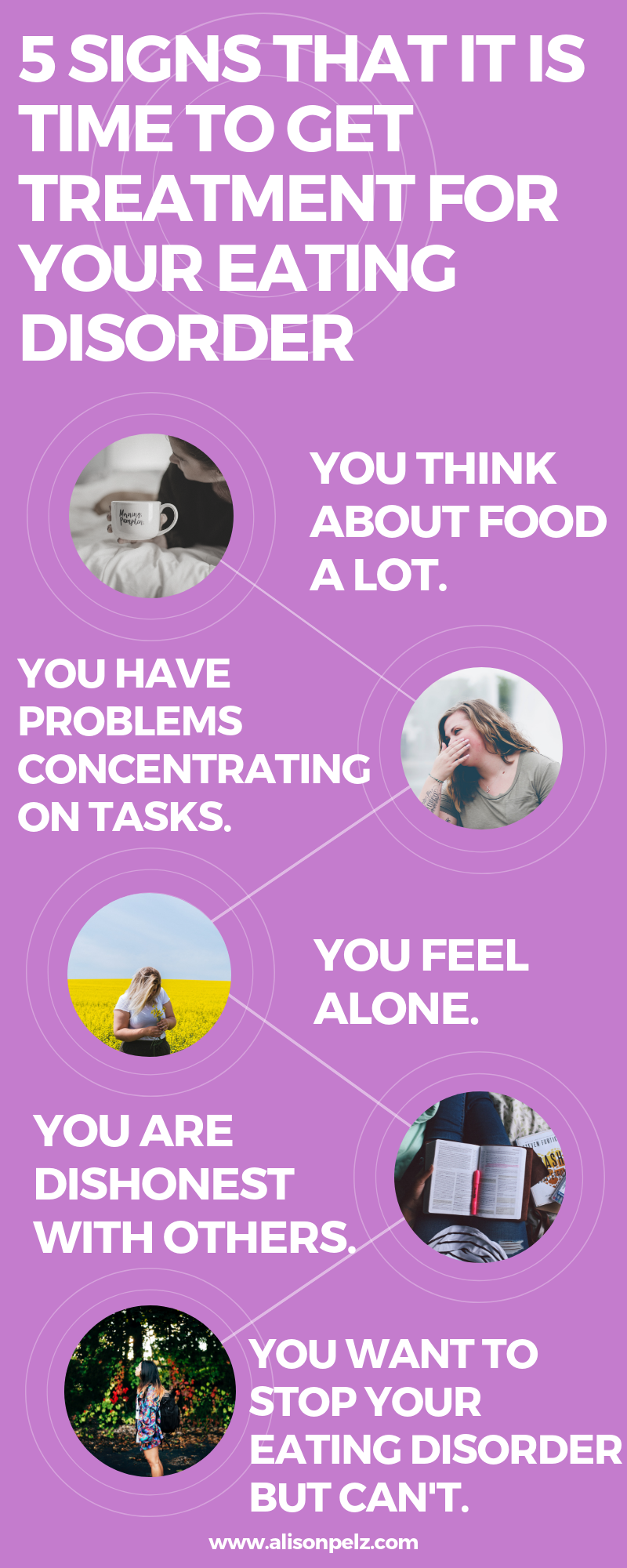
4. Stay curious about your eating disorder symptoms.
Your eating disorder symptoms may change, or they may wax and wane during this time. Try to refrain from being judgmental about your eating disorder symptoms.
Instead, ask yourself something like, “I am noticing that I am doing this eating disorder behavior more. What may be going on or what may I be feeling?” Being curious rather than judgmental allows for problem-solving rather than shame.
5. Be as social as you can while physical distancing and stay-at-home orders are in place.
Social isolation and loneliness can affect your physical and mental health. Regularly connecting with family, friends, co-workers and/or classmates via telephone or virtual meetings can help reduce feelings of loneliness. Check with your treatment team, as they may be aware of virtual eating disorder support groups that can help support your recovery during the pandemic.
Your eating disorder recovery may look different than it usually does during the pandemic, and that’s okay. Using the tips above and taking it one day at a time is a good place to start.