Starting a new semester (or starting college for the first time) is associated with many positive feelings and excitement. However, along with these positive feelings, college students may experience feelings of isolation, worry, and sadness that often come along with major life transitions.
Unfortunately, these feelings may worsen eating disorder symptoms for college students who are struggling. When you’re already under stress from school and new social situations, it can be tricky to get a handle on your eating disorder symptoms or to move forward in your eating disorder recovery.
Why is it hard for college students to maintain eating disorder recovery?
Increased demands + independence
Returning to college, or going for the first time is exciting! It’s often a breath of fresh air to see friends you haven’t seen all summer, move into your new home for the year, and get into the swing of a new semester of classes. The taste of freedom and independence that college offers is hard to beat!
If you have already experienced some time at college, though, you know that gaining independence also means more responsibility–which at times can be overwhelming. If you’re attending college for the first time, it’s normal to feel both excited at the opportunity for independence and totally overwhelmed by what that independence means.
It can be challenging to set boundaries for yourself while managing-the demands of being a student, your social life, caring for yourself, and recovery. Increased demands often mean increased stress, which often is associated with an uptick in eating disorder symptoms.
Changes in Routine
When in recovery for an eating disorder, changes in routine can be tough to deal with. Routines allow for some comfort and dependability. When we have a routine, we know what to expect and when to expect it. It cuts down on the level of uncertainty or stress we feel about the unknown. College students often find that it takes a few weeks or longer to figure out their new routine.
Routines also have very practical uses in recovery. They affect meal planning, treatment appointments, sleeping habits, and more, all of which play a role in recovery! Navigating a new routine can be challenging, and can feel overwhelming. Giving care and consideration to what your new routine will be and how it works for you is important.
Diet culture on Campus
On a college campus, you’ll be surrounded by other young people, who are also surrounded by the constant messaging on social media about diet and beauty standards.
Gyms on campus may be full of college level athletes training in ways that other folks who don’t need intense conditioning for a sport shouldn’t be pushing themselves to compete with.
You might be surrounded by fear of the “freshman fifteen”, or feel pressure to skip meals to study for exams with other students. The culture around food and exercise on a college campus may not be the healthiest one. It’s important to prepare for that with a counselor beforehand so you have coping mechanisms you can use when the need arises.
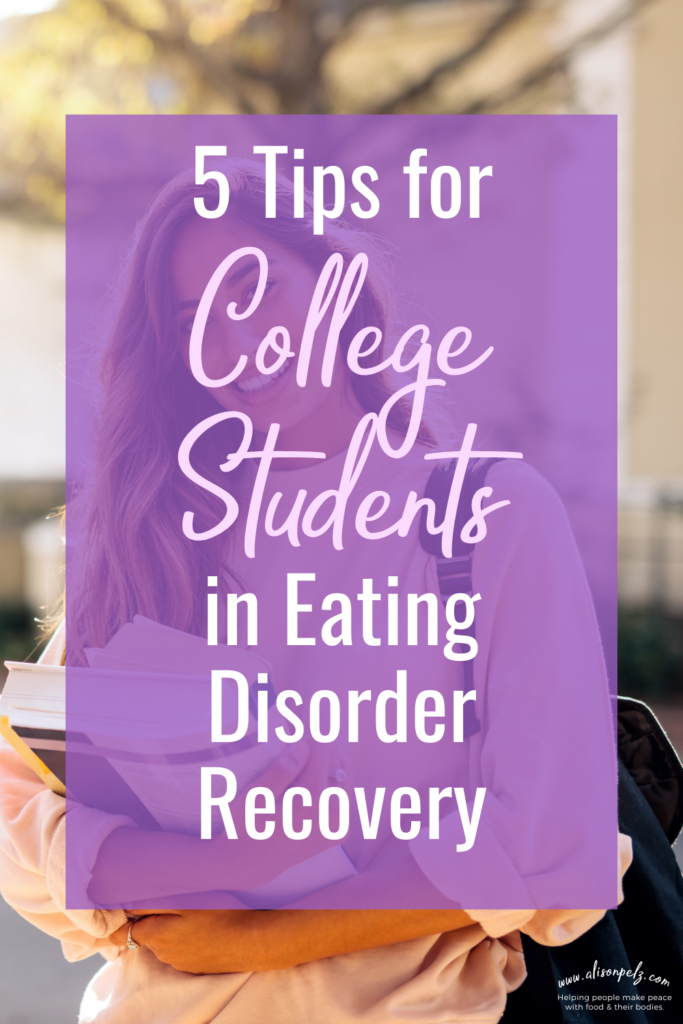
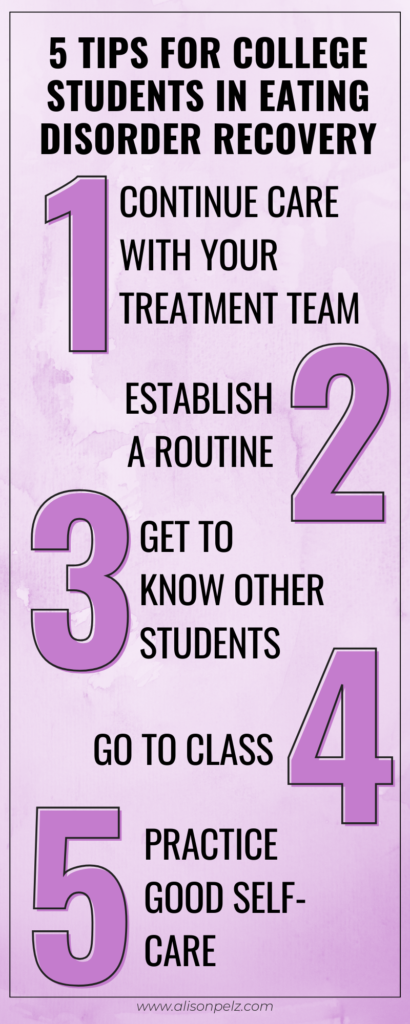
Are you wondering what you can do to support eating disorder recovery at the start of a new semester? Here are 5 things college students can do to stay on track with eating disorder recovery.
1. Continue care with your eating disorder treatment team
It’s important to continue the work you’re already doing with your eating disorder treatment team as you transition back to school. The start of a new semester means a changing schedule, routine, and living situation in many cases. Making sure you have the support of your treatment team can help you weather these changes so you can have the best experience possible at schoo.
If you don’t have a treatment team a good place to start is your college health center. Most colleges don’t provide long-term counseling for eating disorders, but they can put you in touch with providers in the community that can support you throughout the school year so you can get the help you need.
2. Establish a routine
Remember, routines help us all, but they especially help folks with eating disorders. Routines give us peace of mind, comfort, and help us stay on track with eating, which is a crucial part of recovery.
Just as I am sure it took some time to establish a summer routine, it will take a bit for you to establish a school routine as you find what works for you and your needs. Be patient with yourself!
3. Get to know other college students
Support is crucial in recovery, not just from your treatment team but from the people you care about. It’s easy to get so into your school routine that you forget about reaching out to your friends regularly. Make sure to check in with yourself often to see if you are getting enough socializing in (or if you are getting too much – alone time is also important for self-care).
If you are new to campus or find yourself feeling isolated consider joining a club. Most campuses have tons of clubs and organizations that cater to a variety of interests and skills for college students. Consider joining a club for fun and a club that has to do with your major to start with so you meet a good mix of people from inside and outside of your academic department.
4. Go to class
This may sound like a no-brainer. But, it feels like since the pandemic more universities still have a fair amount of classes online. If you have a choice, consider taking all of your classes in person. We’ve done enough online for the last two years. It’s also hard enough to concentrate at times, especially in the middle of a lecture, and it can be even trickier to focus when you have all the distractions of home around you.
Actually stepping foot in the classroom can help you get more in the school mindset, and it can also be a great way to meet other college students.
Additionally, I know it is very enticing to skip classes at times (after all, most professors don’t take an attendance grade). It’s always tempting to get a few more hours of sleep or to use your time for something else, but skipping class has some drawbacks. Missing classes often makes us feel more depressed, isolated, and guilty instead of relieving stress.
5. Practice good self-care
What’s your self-care routine? It’s important to remember that you’re worthy of being taken care of. Self-care can include getting your nails done, taking a hot bath, or using a face mask. It can also include things like getting enough sleep, taking your medication, setting boundaries, and having hard conversations.
We often have an idea of self-care as fun little treats or splurges, but self-care isn’t only about spending money. It’s about taking care of your emotional and physical needs.
Self-care can mean different things at different times. Sometimes it might mean decompressing by yourself in front of the TV. Other times it might mean making time for friends and social events with other college students. Try to check in with yourself regularly and ask what your self-care needs are at the moment. Remember, it’s not selfish to take care of yourself- it’s necessary.