 Chronic dieter? Feel out of control with food? Tired of weight cycling? Feel guilty after eating “bad” foods? Feel at war with your body? Concerned about your health?
Chronic dieter? Feel out of control with food? Tired of weight cycling? Feel guilty after eating “bad” foods? Feel at war with your body? Concerned about your health?
If you answered “yes” to any of these questions, I highly recommend reading and learning about Intuitive Eating developed by Evelyn Tribole, MS, RD and Elyse Resch, MS, RD, FADA.
The first edition of Intuitive Eating was published in 1995. For over 15 years, I have been using principles of Intuitive Eating with clients. Recently, I trained with Evelyn Tribole, MS, RD to become a Certified Intuitive Eating Counselor. I am excited to share the ins & outs of Intuitive Eating & other tools, over my blog, webinars and in one-on-one sessions.
Intuitive Eating is an evidence-informed approach to making peace with food used by counselors, dietitians and eating disorder treatment centers across the country and worldwide.Continue reading

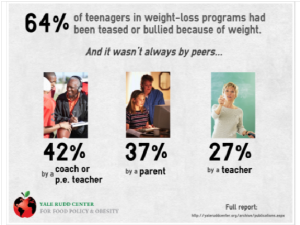
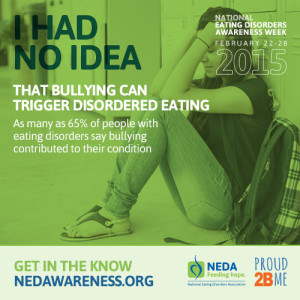 l know that bullying is harmful to our children. And researchers and eating disorder professionals are now just starting to understand that bullying can contribute to disordered eating. If a pre-teen or teen has an eating disorder they could be using their eating disorder behaviors to cope with being bullied. To read more about how disordered eating/eating disorders are believed to be “helpful” in coping with life stresses please visit
l know that bullying is harmful to our children. And researchers and eating disorder professionals are now just starting to understand that bullying can contribute to disordered eating. If a pre-teen or teen has an eating disorder they could be using their eating disorder behaviors to cope with being bullied. To read more about how disordered eating/eating disorders are believed to be “helpful” in coping with life stresses please visit 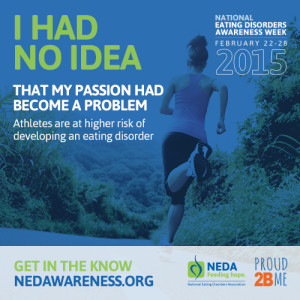 22nd, kicks off
22nd, kicks off