There’s a lot of buzz in the wellness and mental health worlds about body positivity and body acceptance, but what do those terms even mean?
Body acceptance is the idea that it’s not always possible to feel positively about your body, but it is always possible to accept it and treat it with kindness. The end goal of both of these is to increase the acceptance of all body sizes and to help people feel more comfortable in their own bodies.
In contrast, body positivity is the idea that everyone deserves to feel positively about their body image. If you’ve ever seen a post on social media telling you to “love your body”, then you’ve probably experienced body positivity.
At first glance, body positivity sounds great. After all, things would be so much simpler if we could all just love our bodies! However, that’s often easier said than done for a number of people.
The idea of body positivity has its roots in fighting diet culture, but the term doesn’t resonate with everyone. After all, feeling positive about your body is a tall order for a lot of people.
First of all, there is a multi-billion dollar diet industry that uses its considerable resources and influence to convince us all that there is something wrong with our bodies. Feeling insecure about how our bodies look is a surefire way to get us to buy products that will “fix” us. However, consider the idea that there was nothing wrong with your body in the first place.
People who are chronically ill or have varying abilities might not feel like they can be positive about a body that is constantly in pain or not able to move through the world easily. People who are recovering from eating disorders might not trust their body’s cues or might feel distress when thinking about their bodies.
Body acceptance might feel like a more attainable goal than body positivity.
You might also go back and forth between positivity and acceptance for your body depending on the day. Nothing lasts forever, and the feelings you currently have about your body probably won’t last. What will last are the consequences of the way you treat yourself, so do what you can to show yourself compassion.
It’s important to remember that one isn’t better than the other. Body positivity and body acceptance are options, and if one feels more attainable than the other, don’t push yourself to feel things about your body that you’re not ready for.
Here are some questions that I get asked frequently about body positivity and acceptance:
Question: I hear all of this stuff about body positivity and feel hopeless. I feel like I am nowhere near loving my body. Is it necessary for me to feel body positivity to recover from my eating disorder?
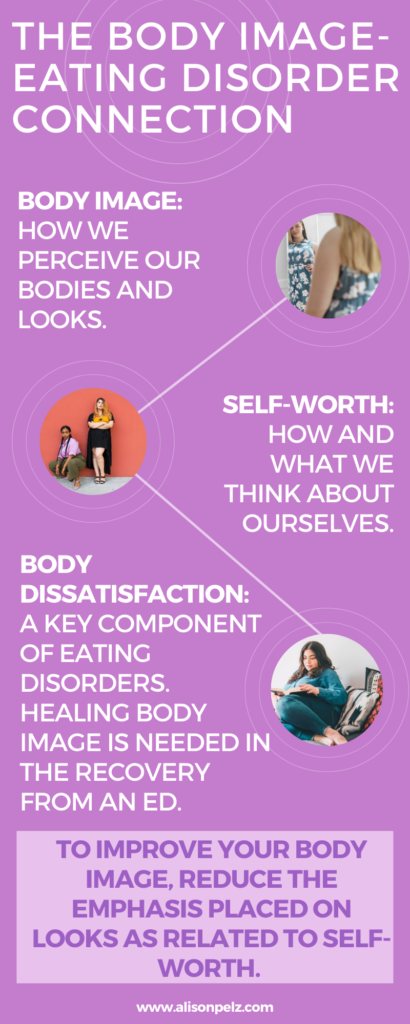
Answer: While body image, or what we feel and think about our body, is closely tied to eating disorders, body positivity is not necessary for recovery. Body positivity is an ideal outcome of recovery, but it’s not the only outcome available.
In a nutshell, body dissatisfaction or a negative body image often contributes to the extreme eating and exercise behaviors we see in folks with eating disorders. In fact, if negative body image is not in check, the eating disorder will keep going. However, feeling positive about your body is not required to start recovery.
Body acceptance is often a more accessible place to start. As mentioned above, body acceptance is the practice of acceptance, even if you aren’t completely satisfied with it. Body positivity is the practice of feeling positively about your body, which can be a lot harder to do.
It is okay to like some parts of ourselves, but not all. Like so much in life (jobs, school), we may like some parts but not all. Either way, we accept that the parts we don’t like are there.
Question: I really don’t like my body. How can I at least work on increasing body acceptance?
Answer: The knee jerk reaction in our culture is if we don’t like something we need to “fix it”. Certainly, diet culture gives a false notion that if we “work hard enough” then we can have the body we want.
I am here to say I have never met a person with an eating disorder that is NOT a hard worker.
Body acceptance is about changing our thoughts about our body, not about changing our body to match our thoughts.
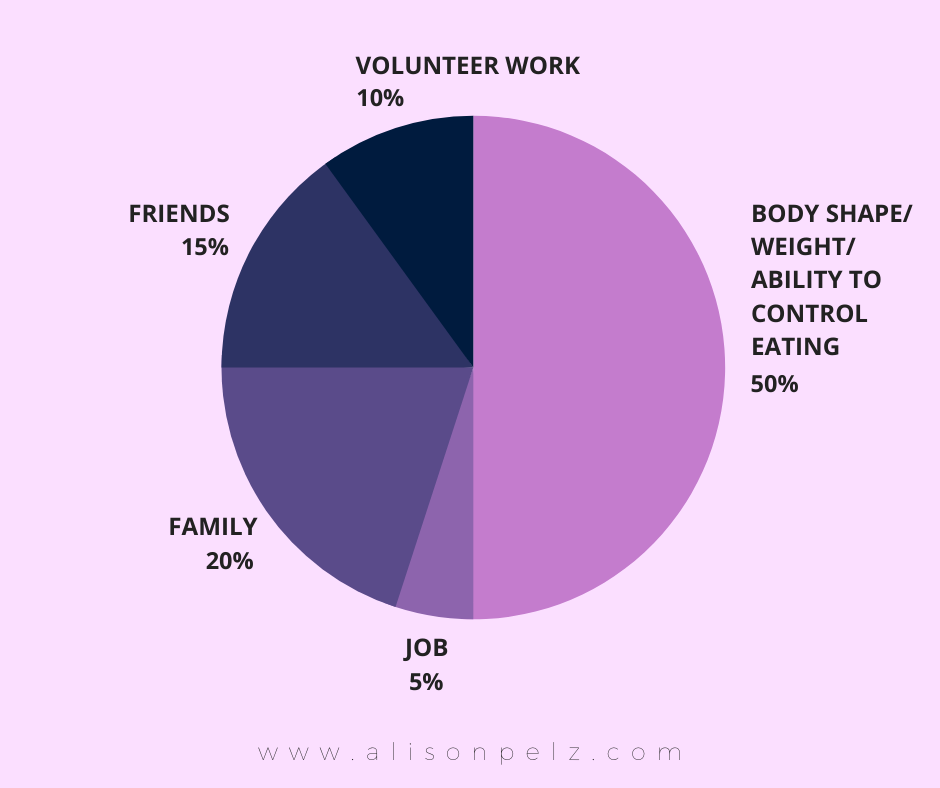
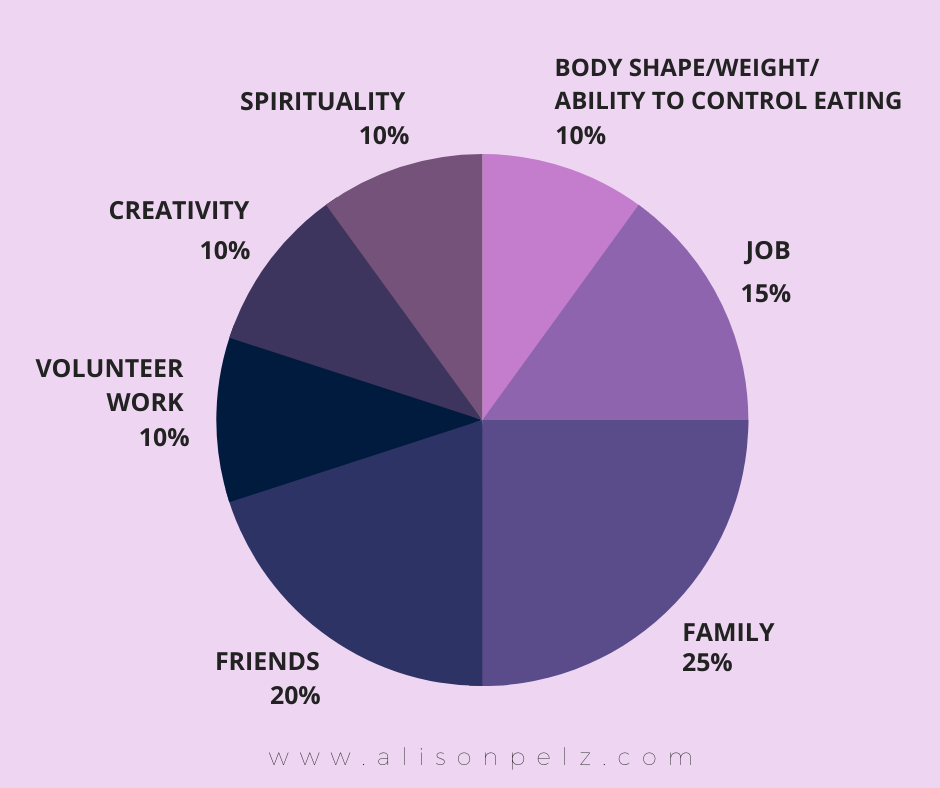
A typical thought someone may have with body dissatisfaction is “If I get my body to look a certain way I will be more confident.”
While there may be some truth to that, changing your looks is not the only way to feel confident. Confidence can come from so many places, but unless you address the root of that insecurity, a new one will pop up in its place.
If you broaden your thoughts, you will see that there are lots of other ways to build or have confidence without staying in your eating disorder.
Another typical thought someone may have about body dissatisfaction is “I am afraid of what people are thinking of me.”
That is to say you fear people will react negatively to you. Lots of times, you don’t even have proof of this happening, but the fear is there all the same.
Unfortunately, many folks who struggle with eating disorders have been teased, ridiculed, or bullied about their body. Many people who struggle with eating disorders come from families that place high value on looks. (If that’s the case for you, this is something to address and unpack with a therapist.)
More often than not, when we assume people are thinking something bad about our bodies, we don’t have any evidence to back this up.
These thoughts and worries are the real distress, not our bodies. Freeing yourself from the worry that other people are judging your body can give you more time to think about what it would feel like to accept your body as it is.
If accepting your body still sounds scary, there are things you can do to help. One way to increase body acceptance is to identify parts of your body that you do like. It is OK to like some parts of your body but not all parts. You can keep a journal where you write down what you like about your body. You can write down something that you’re grateful for that your body does – like how your stomach holds in all your organs and protects them, or how your thighs help you get from place to place. You don’t have to love each little bit of your body to want to take care of it and keep it safe. Acceptance is enough.